Who Did You Bring with You Today?
Friends and family aren't the only ones who accompany patients to their appointments.
One of the most painful blunders that I have made in an exam room is addressing a young woman accompanying an older male patient, “Oh and is this your daughter?”
The correction (“I’m his WIFE!”) is cringe-inducing. Not the best first impression and pretty much sums up the mantra “you know what happens when you *assume* something…”
After watching me make this mistake several times, my nurse gently shared how she approached a new patient with a guest in the room. She always asked, “And who did you bring with you today?’” she told me. It gave the patient the chance to name the relationship, so she didn’t have to guess. This was a brilliant suggestion and I’ve been using it ever since.
A few years back, my nurse called me back to our CT scanner. A patient was in severe distress and despite their best efforts, she and our radiation therapists needed me to make the call on cancelling his scan. I had seen the man in consult the week before and he appeared normal. He asked appropriate questions and was relieved when I told him that our intent was to cure his cancer. After a pleasant conversation, we shook hands, and he headed to the front desk to schedule his planning scan. I could not imagine what would have upset his calm demeanor.
When I arrived, my patient was sitting on the CT scanner table, and I could feel the tension in the room. The therapists were frustrated and upset. As I got closer, the patient was drenched in sweat. “I can’t do it,” he said, shaking his head, “I just can’t have that thing over my face.”
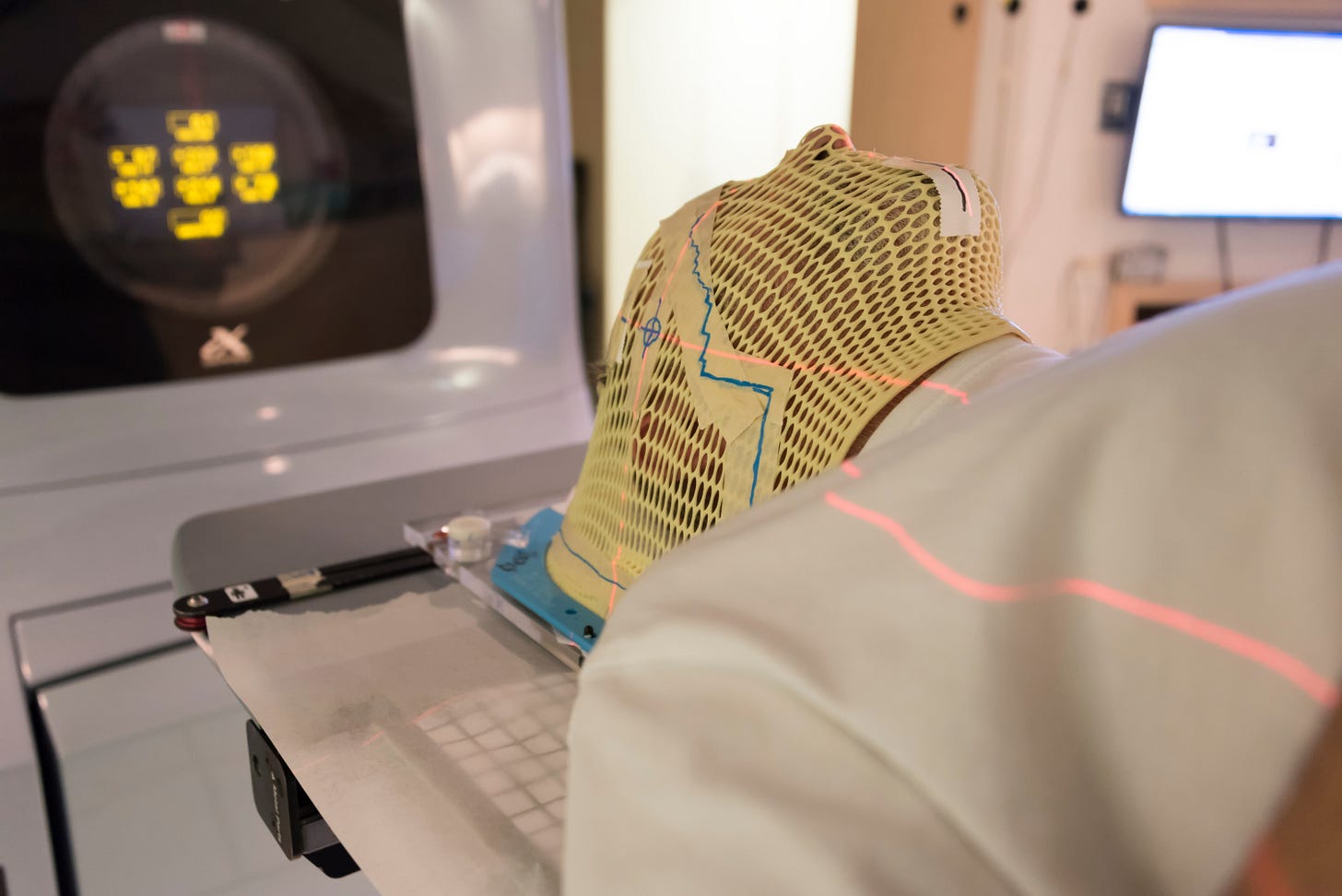
Radiation masks are made of tight fitting, plastic mesh. It’s possible to see and breathe through the holes but many patients understandably experience stress as they hear and feel the plastic clips snap into place. Their head is attached to the table and there is no way for them to escape.
With time (and sometimes by cutting holes for eyes), most patients are able to tolerate the feeling for the 5-8 minutes it takes to complete their treatment. They power through but I’ve yet to hear one who would want to go do it again.
We need the mask to be tight so patients cannot inadvertently move their heads. Even a 5-millimeter shift risks placing critical normal structures in regions of very high doses of radiation. The target areas for tonsil cancer treatment, for example, are in what I call “high price real estate.” The hearing apparatus, brainstem, jaw, spit glands, and optic structures are very close the patient’s tumor. We can be more precise and have less of a chance of damaging these normal structures (and causing long term side effects) with patients’ heads immobilized in tight masks.
I started to explain this reasoning to the man, but I could tell he wasn’t hearing me. I pulled up a stool and asked what he was feeling when the mask was on. He told me that he had never liked tight spaces. That he was terribly claustrophobic, and the mask exacerbated this feeling. He apologized profusely and reiterated his desire to get treatment. We agreed to a short-term trial of anxiety medication that he could take before his treatment. He left relieved.
He returned the following week and, with medication, was able to complete the scan and start his treatment. At one of our weekly meetings, I asked whether he now felt that he could tolerate treatment without the meds. He surprised me when he jumped out of his chair and started pacing the floor, fists balled at his side.
He started talking animatedly about his childhood. He had grown up in abusive home. His mom worked so his slightly older sister was left to care for him. “When I was bad,” he told me, “My sister would put me in the clothes dryer and turn it on. That mask makes me feel like I’m in the dryer again. I don’t like to feel like that.”
I didn’t know what to say.
Of course, the mask reminded him of the punishing space he’d been locked in as a child. Of course, he felt helpless when he realized that he could not escape. We were not just treating the middle-aged small business owner who paced in front of me. The toddler inside him remembered the terror of his family’s cruelty.
I thought about him through the years when patients had reactions that seemed out of proportion to the challenge in front of them. He was not alone in bringing someone else to his treatments with him.
One woman cried every day - from the time she walked in the treatment room until the treatment was over. I asked about it once, wondering if I had missed something or if we had done something wrong. She shook her head, embarrassed. She loved the radiation therapists and everyone was so kind. She understood she had a great prognosis and was feeling well.
Because of my previous patient, I asked her about her childhood. She paused for a long minute and started crying.
Her mother died when she was 10. “I know she had cancer, got radiation and died” my patient shared, “but I don’t really know what happened to her. No one talked to kids back then. All I remember is her lying in bed and my father telling me to play quietly so that she could rest. And then she died.”
It wasn’t until I was working with my own therapist that I was introduced to the Internal Family Systems (IFS) model. Created by psychologist Dr. Richard Swartz, IFS suggests that our minds are made of distinct “parts“- each with its own unique qualities and viewpoint. These parts can be healthy or unhealthy and can be forced into extreme roles by life events or trauma.
IFS trained therapists encourage their patients to talk to these parts and listen to their needs and desires. By acknowledging what the part is trying to accomplish, we can choose whether to listen to that part or not.
After learning about IFS, I wondered if my patients’ childhood “parts” were trying to protect them. In the case of my male patient, did the part feel like he was back in the dryer as my patient suggested? Or in my female patient, was her 10-year-old part missing her mom but trying to be quiet?
This week, I saw a patient who had been treated for cancer many years ago. She acknowledged that she was having a difficult time adjusting to her second diagnosis after so much time had passed. She thought she would be “better” at it. She chastised herself for “letting her guard down,” for not remaining on high alert as if that would have prevented this unrelated cancer from forming.
We talked about the impact of her cancer thirty years ago, about her life as a young wife and new mother that had been interrupted by a life-threatening diagnosis. I suggested she write down her thoughts. I offered a referral to our family support team, and she agreed to consider it.
I am not a therapist and although I’ve read Dr. Schwartz’s excellent book, I’m not trained in his technique. It is worth considering, however, who we are bringing with us - in to an exam room, into cancer treatment, into a new job or into a relationship. Is there a “part” that is dictating our feelings, reactions or actions in a particular setting? Is part of our past is trying to speak to us in that moment? What is she/he saying? Is this reaction helpful or not?
Who have you brought with you to that moment and what are they trying to tell you?
On my mind…
The evidence is overwhelming that there is no benefit to any amount or type of alcohol.
If cancer prevention or remaining cancer free is your goal, you would be wise to consider giving it up completely.
But what are the alternatives?








A very thoughtful piece. Thank you!
Appreciate these poignant examples ❤️