The largest cancer meeting in North America just wrapped up. Held annually in the spring. the American Society of Clinical Oncology meeting is where big advances and promising discoveries are announced. This year’s highlights included a study that showed that moderate exercise improved survival in colon cancer patients as much or greater than many chemotherapy agents and that treatment for breast cancer could be modified based on levels of cancer DNA circulating in the blood rather than waiting for spots to show up on an imaging test.
In reflecting on these findings, oncologist
pointed out a flaw in how we talk about “success” in clinical trials. Overall Survival, for example, measures if patients are alive or dead. Progression-Free Survival measures if patients are alive with their cancer controlled or uncontrolled. The endpoints that researchers typically use are binary and designed to counter ambiguous interpretations. These yes/no answers, however, condense complicated scientific questions into concrete endpoints. This is useful for regulatory bodies like the FDA to make decisions about approving a drug treatment for routine clinical use.Most of us would agree that being alive is better than the alternative. However, patients surviving cancer often have a more nuanced view. Many of my patients begin conversations with statements like “I want QUALITY of life” or “I don’t want to suffer.” A rubric to incorporate these wishes does not exist. Would a patient, for example, trade a better quality of life for a 20% less chance of cure? 10? 5?
Today, I invite you to listen in on a conversation that I had with two cancer survivors. Both Mark and Yvonne are alive and cured. In our professional parlance, they would be considered success stories. And as you hear them talk about their lives after cancer treatment, they are living.
But they are living with life-changing side effects. You will hear about how large chunks of their identities disappeared in the aftermath of cancer treatment. These sacrifices are part of the hidden cost of cancer that is not often discussed (and certainly not used for approval) of new treatments. Years after their last treatments, they have accepted their “new normal” but aren’t satisfied. They want better treatments for those diagnosed now.
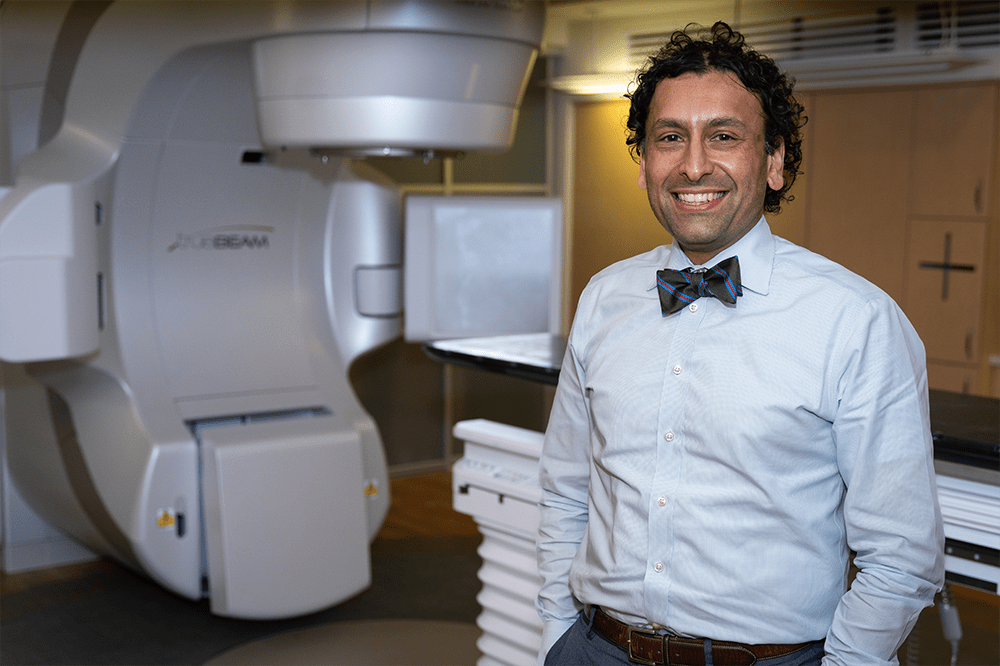
Afterwards, I talk with a colleague, Dr. Bhisham Chera, about his groundbreaking work in studying less toxic ways to treat patients like Mark and Yvonne.
I’m not sure, however, that we should be throwing these trials out. Would I, for example, be willing to sacrifice a 5% increase in the chance my cancer would return if I had a better chance of being able to taste food for the rest of my life? Perhaps. But right now, I wouldn’t have that choice. It would be considered unethical to even discuss it.
Enjoy and I look forward to hearing your thoughts in the comments.
Yvonne McClaren is a patient advocate and writer helping people recover from radiation-induced dysphagia with dignity and practical, real-world strategies. Her signature 8-week food reintegration program, Eating Together Again, is designed for both head and neck cancer survivors and the speech-language pathologists who support them bringing confidence, connection, and joy back to the table. Start here: www.yvonnemcclaren.com.
Mark Kalstrup is almost 7 years post treatment. “The gift that cancer afforded me is to approach each day as a new beginning and to assist others by inspiring hope for tomorrow.”
Bhishamjit Chera, M.D. is a board-certified radiation oncologist, Vice Chairman for Safety and Quality Assurance in the Department of Radiation Oncology, and the Wendy & Keith Wellin Endowed Chair in Radiation Oncology.
He is nationally and internationally known for his pioneering work in evaluating reduced intensity radiation and chemotherapy treatments for patients with human papillomavirus (HPV) associated with throat cancers. He has also co-invented a blood-based biomarker for HPV-associated cancers.
















Share this post