What You Don't Know About Cancer Staging
Be careful what you ask for when lobbying for another scan.
One of the most terrifying experiences of my teenage life was teaching kindergarten Sunday School. A friend and I, desperate to escape our awkward high school youth group, signed up to teach a summer session. The first time I yelled, “Tyler! Stop hitting Lauren with the Bible!” I realized that early childhood education was not for me.
The wide range of social and physical developmental stages expressed by our 5-year-old charges surprised my teenage self. One child recited ‘Twas the Night Before Christmas from memory while another struggled to stack blocks on the floor. Some still wore diapers while others took themselves to the bathroom down the hall. Thankfully, we all survived that summer and I hope a dad somewhere still cherishes the pasta encrusted picture frame commemorating Father’s Day 1994.
“What stage am I?” is an important question that helps patients get their bearings in the initial confusing stages of workup and treatment planning. Cancer staging provides a place on the starting line, a measure of where they are in comparison to others in similar situations. Staging also allows doctors and researchers to group similar patients together in order to communicate with each other about general prognosis and standard treatments.
Stage IV, for example, usually denotes metastatic or incurable cancer. Like my Sunday School charges, however, all Stage IV cancers are not the same. Cancer is different in every individual. If that makes cancer staging sound as unhelpful as elementary school grades, it’s true. But for now, it’s the best we’ve got. As Winston Churchill said about democracy, “No one pretends that democracy is perfect or all-wise. Indeed, it has been said that democracy is the worst form of Government except for all those other forms that have been tried…”
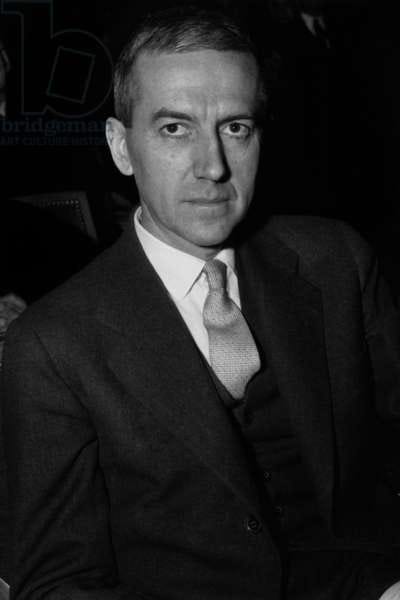
French surgeon, Pierre Denoix, is credited for developing the first staging system. Described as “Nomenclature Classification des Cancers” by Dr. Denoix in 1944, his TNM staging system provided a simple method for classifying breast cancer based on the size of the tumor (T), involvement of any lymph nodes (N) and presence of metastases or cancer in the rest of the body (M). In rough strokes, Dr. Denoix and other surgeons like him used the staging system to figure out which groups of patients benefited from radical mastectomies for breast cancer. Within a few years, the international cancer community adopted Denoix’s TNM staging, and it forms the basis of cancer staging today almost a century later.
The 8th edition of the American Joint Committee on Cancer (AJCC) staging manual provides staging forms for 45 sites of cancer using classic information like the TNM staging as well as more specific determinants of tumor behavior. This guide stratifies patients into numbered groups based not only on the physical location of cancer but by using other important information like the presence of genetic mutations, blood levels of certain molecules and even, in the case of head and neck cancer, the presence of virus particles like HPV (human papillomavirus). The main driver, however, continues to be where cancer is in the body. I use these useful categories to determine treatment of similar cancers every day.
Proper classification and staging of cancer will allow the physician to determine treatment for the patient more appropriately, to evaluate results of management more reliably, and to compare statistics reported from various institutions more confidently.
- Oliver H. Beahrs, MD in the first edition of the cancer staging manual.
As we get better at figuring out where cancer is, however, we have to be careful. A recent trial published in the Journal of Clinical Oncology looked at the impact of adding a PET scan to staging in advanced breast cancer patients. Half of the patients got a PET scan in addition to standard studies like a bone scan and CT scans and half did not. The study found that PET scans found additional areas of cancer in about 10% more patients than standard imaging alone. That sounds good right? The PET scan found more cancer. Not so fast. Finding this additional cancer led to upstaging 22 patients from curable to incurable aka Stage IV.
Interestingly, the patients who had PET scans also had more biopsies, more follow up imaging and were less likely to receive aggressive treatment than patients who received standard testing. In the accompanying editorial, experts wondered if finding these small extra islands of cancer cells was “worth it”. By finding microscopic areas of cancer, had patients who were potentially curable been robbed of that opportunity? Did the extra costs and painful procedures help?
Scientists estimate that it takes 100K to 1 million cells getting together before we can detect them on the best PET scan. Often chemotherapy is given after surgery because we assume that in high-risk patients, even if we can’t see them, there are collections of 100s of cells in the body that are hiding out. Chemotherapy, delivered by the blood stream all over the body, kills these cells and cures the patient. The question becomes when does chemotherapy work? At 100 cells? 1 million? Where do we set the bar for “cure”?
More information sounds like a good thing but in some cases, it may not be helpful and in fact might be harmful to your care. I explain it to my patients like this: more information is helpful only if it’s helpful information. You can tell me your favorite ACC basketball team, for example, which gives me more information about you, but it is not helpful in determining care of your cancer. In fact, I might have to tell you to seek care elsewhere if you tell me you are a Duke fan. :-)

Patients are understandably desperate to determine their fate. They want to know as much as they can to answer the basic question: What are my chances? PET scans as a part of staging at least in breast cancer may help answer the question of where cancer is but may also inadvertently cause patients who may have been cured to be placed into an incurable treatment group. So, when a patient begs me to order a PET scan, most of the time, I respond with the question “What information are you missing?” Often, the answer to that question will not be found in an imaging test.
What is your experience with pushing for scans? Did you find the information you wanted or the diagnosis that eluded your doctor? Or not?
On my mind…
I enjoyed this HBR article explaining how organizations respond to change. Social defense responses preserve traditions and resist outside ideas to the detriment of the company. You may be familiar with the phrase “That’s now how we do it here.”
I was honored to write the foreword for The Long COVID Reader, an anthology of works exploring the challenges of living with Long COVID. If you know someone who suffers from Long COVID, you can find out more about the book here.
My friend and colleague, Susan Yaguda, spoke on a podcast recently about the evidence-based benefits of music therapy in addressing distress in cancer patients. We have to stop thinking of integrative therapies as nice add-ons and instead actually integrate them into standard care.




And just to add more confusion, brain cancer is graded not staged cuz why keep things simple?
ahhh scans, the clunk of the MRI for head and neck. They scanned me and some idiot ( I can call her that here) who had no right to tell me anything rang me with scan results saying the treatment had not worked as well as they would have liked. She was wrong. Enough said. Good post