Let's Have a Baby! Or not...
After a cancer diagnosis, how long do we have to talk about the future?
Lauren Tarpley’s breast cancer was found when she sought medical care for an unexpected pregnancy loss. Lauren and her husband had been trying to conceive for several years. At 34, the dual devastation of cancer and miscarriage was almost more than she could bear.
The day before she started chemotherapy, Lauren underwent an egg retrieval procedure and was able to freeze embryos fertilized by her husband’s sperm. In her mind, the possibility of IVF using these stored embryos was a safety net. During chemotherapy, she also received shots (Zoladex) to protect her ovaries with the hope that she would be able conceive naturally after her cancer treatment was over. The fertilized embryos were there just in case.
She shared her pregnancy story on The Burn podcast:
It appeared that my Zoladex hadn't protected my ovaries from the chemo like we had hoped. My egg quality was very bad and barely registered. I was told that I was premenopausal and my only chance for more children was via IVF using the embryos we had frozen prior to treatment. She also told me that since my cycle hadn't returned it likely wasn't going to return.
When I received this information, I was torn, and I was shocked. I was relieved that I had done IVF, but I was shocked that this was the outcome. I didn't want to disappoint my family again. They had been with me through it all. My husband, especially, he wanted me to be healthy and whole, but he also wanted another child.
I took a day to grieve that loss, and I woke up the next day determined. I called my nurse and planned out the schedule for IVF and implantation.
I encourage you to listen to the rest of her amazing story.
Dr. Will Flanary, an ophthalmologist and medical comedian who goes by the name “Dr. Glaucomflecken,” is a two-time testicular cancer survivor. His wife, Kristin aka “Lady Glaucomflecken” spoke about the moment they received the diagnosis that he would have to have his second testicle removed on the It Takes Balls podcast:
It took a while to wrap our mind around it and then it came with a lot more consequences for us. Again, he only had to have surgery and that was great that he didn’t need radiation or chemo, but it did mean hormone replacement therapy and it meant infertility.
These are only two stories of the tens of thousands as young adults must make multiple life-altering decisions in a very short amount of time. Both of these couples had “happy” endings to their stories. They are also fortunate in that their physicians discussed fertility with them.
Grouped together and called “AYAs” by the cancer world, about 90K people between the ages of 15 and 39 are diagnosed with cancer each year in the United States. Globally, that number is over a million.
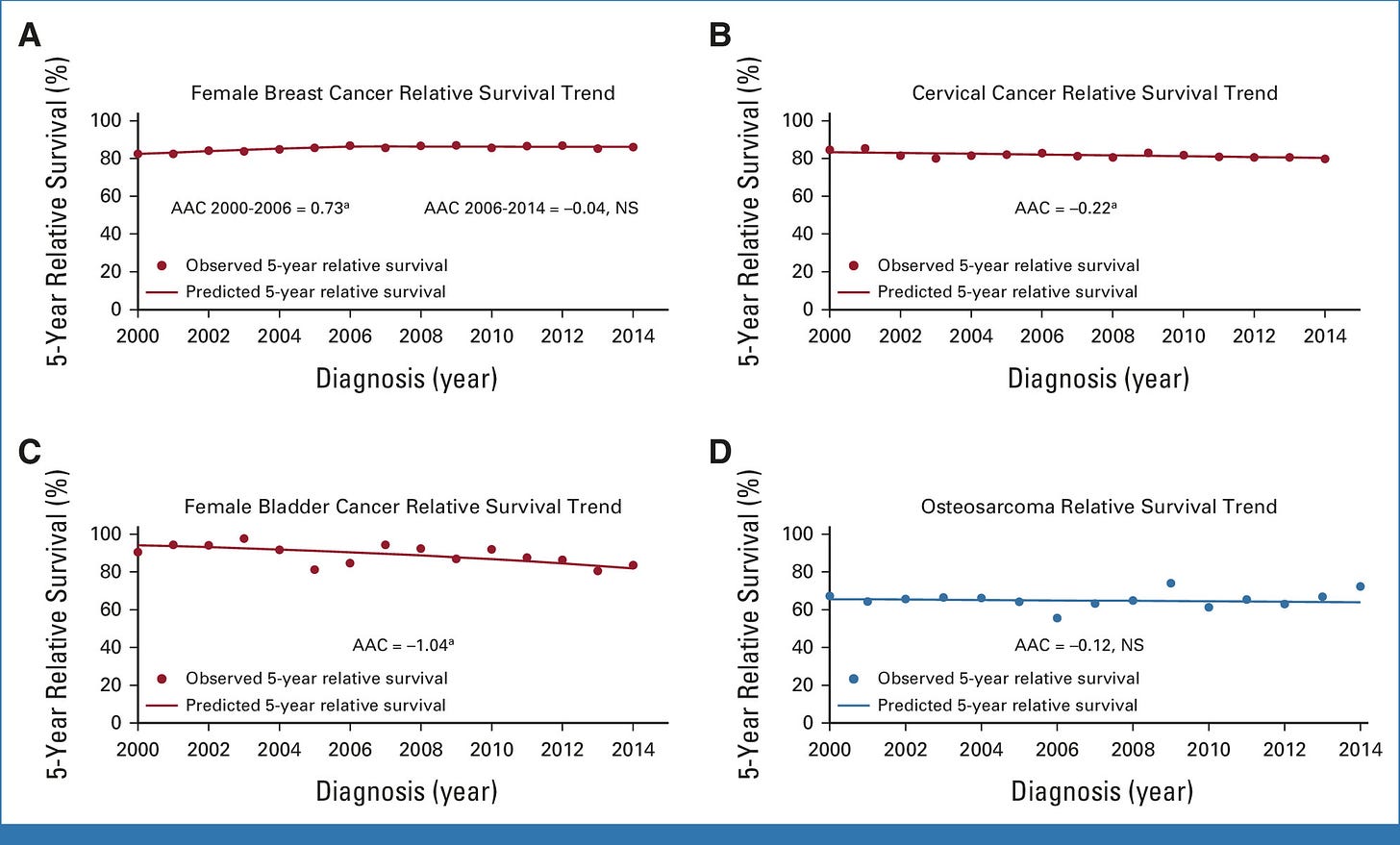
Until recently, the overall survival rate for this group had remained stagnant, but recent studies showed that survival rates are improving with an average 5-year survival of 86% (compared to 64% in older adults).
The most common AYA cancers – Hodgkin and Non-Hodgkin Lymphoma, testicular, melanoma, thyroid and breast cancer - all had a survival rate of >85%.
Whereas colorectal cancer, AML, and osteosarcoma continue to have survival rates of 60% or less.
Cancer treatment administered during the peak reproductive years can cause irreversible infertility. Discussing this life altering consequence and implementing mitigation strategies for addressing it is a critical piece in providing evidence-based care to AYAs. Children diagnosed before puberty don’t have fertility preservation options because they’re not yet producing mature sperm or eggs.
The conversation about reproductive options is fraught particularly for teenagers and their parents, young adults who haven’t thought about having children, and those already struggling with infertility. In the current political climate, the precarity of fertility services and questions about the storage of unused gametes create further wrinkles during an already high stress situation. The urgency to begin treatment adds additional worry when delays for fertility preservation procedures can sometimes take months.
I was therefore not surprised but disappointed to see a recent update from the REACT study. The REproductive Health After Cancer diagnosis and Treatment Study has followed 473 patients aged 18-42 who were diagnosed with cancer between 2013 and 2021.
The study reported that only half of AYA patients recalled a fertility discussion prior to beginning cancer treatment. Alarmingly, these discussions varied by disease (94% of patients with testicular cancer versus 44% with colorectal cancer) and by marital status (higher among married patients than single patients).
In an interview with The ASCO Post, one of the authors acknowledged that this was inconsistent with standard of care and suggested reasons why:
“Some of the challenges included unfamiliarity with infertility risk after a cancer diagnosis, a lack of resources for providing referrals, and clinicians’ perception of the importance of fertility preservation in females who already have children and maybe aren’t interested in expanding their family or are older, which may have contributed to our findings.
A recent JAMA article confirmed these findings. In a survey of top cancer centers in the United States, almost half of facilities reported that fertility services were either not available or had limited availability.
Shockingly, five percent of respondents said they were not sure if their program even offered fertility consultations.
Even if fertility services are available and discussed, financial barriers prevent many patients from pursuing this option.
The primary investigator of the REACT study highlighted the significant cost associated with fertility treatments which are usually not covered even in the case of cancer treatment:
“The cost of pursuing fertility preservation for patients is substantial—estimated to range between $10,000 and $15,000 for oocyte and embryo preservation and between $500 and $1,000 for sperm cryopreservation—with additional costs incurred for surgical sperm retrieval, as well as annual storage fees or both males and females.
And although health insurers typically do not cover fertility preservation, a handful of states, including California, Colorado, Connecticut, Delaware, Illinois, Maryland, New Hampshire, New Jersey, New York, and Rhode Island, have passed fertility preservation coverage laws.
There are also organizations, including the charity Worth the Wait: Fertility & Adoption Grants for Cancer Survivors (https://worththewaitcharity.com), which provide financial support and educational resources for fertility treatments, adoption, and surrogacy.”
And even when this conversation does happen, pregnancy is not guaranteed.
What I wonder is how many AYAs are out there who didn’t know and who only come to realize later that their options for becoming a parent may be limited. And by choices that were made for them by oncologists like me.
Did anyone talk to you about fertility during your cancer treatment?
More on cancer and pregnancy
In a pregnant patient with cancer, how do you save the life of the mother?
A recent publication from Tufts University suggests that ancient viruses left behind pieces of their DNA in human DNA. These pieces, called HERVs (Human Endogenous RetroViruses), now make up about 8% our genome and are found in the DNA of other primates like chimpanzees and gorillas.
Can I help you?
Last week, I was mucking horse stalls, and my phone rang with an unknown number. Expecting a call from our vet’s office, I answered.