Is There a Cost to Doing Your Own Research?
Time with an oncologist is precious. Do you want to waste it talking about this thing you saw on TikTok?
Many years ago, I met a new patient with a curable cancer of his tonsil. He went to his doctor with a sore throat and a few swollen “glands” in his neck. A few weeks later, he was in my office discussing treatment for head and neck cancer.
I told him about the standard treatment of chemotherapy and radiation for seven weeks. We talked about placing a feeding tube in his abdomen, having a dentist determine if any teeth needed to be removed and scheduling a hearing evaluation. I’d had this conversation hundreds of times and this time was just as bad. I tend to paint a bleak picture because the treatment IS awful.
He heard most of this in a previous appointment with his medical oncologist, so he nodded along. He did not seem surprised when went over the laundry list of side effects including a throat so sore that he would require narcotics to swallow his own saliva and a terrible sunburn.
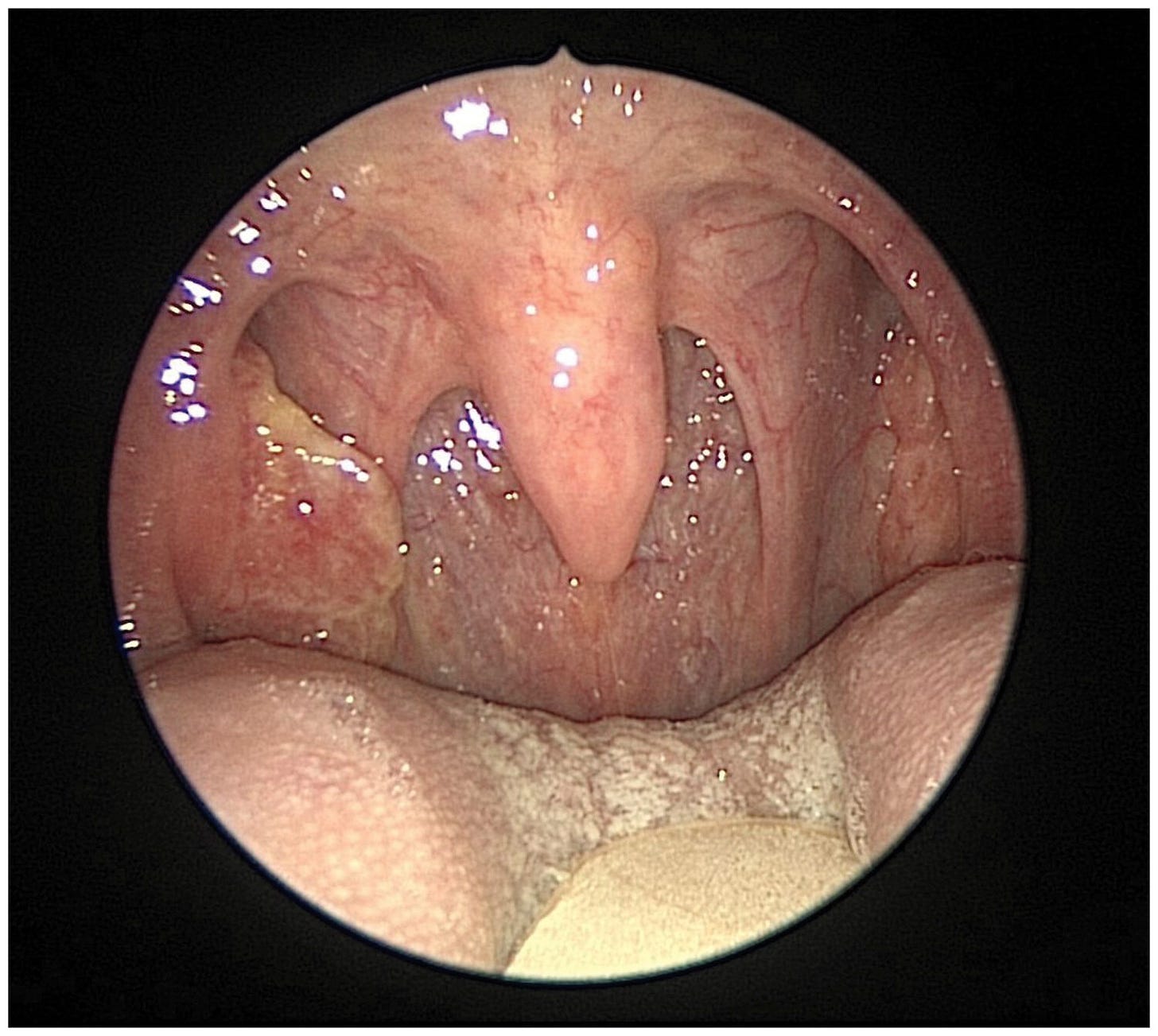
“But his cancer is curable, right, Dr. Wentworth?” his college age son interrupted to ask. I assured him that yes, he had a 90% chance of cure with this treatment, admittedly one of the most difficult regimens in all of oncology.
“We will get you through this,” I promised him, “and we have a team of people who are here to help you. People do this every day. You CAN do this.”
He sat for a moment and then got up. He put out his hand and thanked me for my time. I also stood and shook his hand. I was not sure what was happening.
“I’ve done my own research, Dr. Wentworth. And I’ve got an appointment next week at a clinic in Arizona. They say their treatment is just as effective as yours, but without the side effects. Their treatment will work WITH my body instead of poisoning it.”
He pulled out his phone and showed me the website for a naturopathic clinic in Sedona. The “doctor” there had prescribed weekly insulin infusions along with a cocktail of vitamins. The insulin, he explained, would deny the cancer cells the sugar they needed to survive while the vitamins would boost his immune system to fight the cancer. He told me that he felt sorry for me because I didn’t have this kind of treatment to offer. I looked at his son who sat slumped in his chair, head down.
Still standing, I tried to explain how insulin works and how insulin infusions were not a thing. About evidence-based medicine and fear and hope. He smiled patronizingly at me as I talked and placed his hand on my shoulder. “That’s exactly what they said you’d say,” he said, “Thank you but no. I’m not going to do that to my body.”
His son stood and approached his father. “Please, Dad. Please do what she says.” His fresh, young face was covered with tears.
I spent the night tossing and turning in bed, wondering how I could have approached that conversation differently. How I could have changed his mind. How I contributed to his decision to kill himself in a slow and miserable death.
Three months later, a consult came across my desk one evening. The same patient had been admitted to the hospital. His tumor now involved his tongue and protruded from his mouth. He couldn’t speak or eat. Pieces of necrotic tumor sloughed from his neck. He died of a stroke the next day after the tumor ate through his carotid artery. I never got the chance to see him or his son.
The image of him reaching for my hand, healthy and confident, haunted me again that night. Except this time, I was angry.
Angry at the naturopath who had taken his money in exchange for hope but did not care for him when he died.
Angry that his research prevented him from hearing about evidence-based treatment.
Angry that his son had to watch his dad suffer.
Angry at myself for not having the right words.
I hadn’t thought about him in years until I reconnected with an old friend from medical school. A doctor who specializes in women’s health, my friend lamented that the new patients she saw that day spent their initial conversation with her discussing information they learned from social media. They came to her not to hear her recommendations, but with questions about the treatments these influencers pushed.
“I spend so much time talking about treatments that have absolutely no basis in science, that I don’t have time to talk to them about what will really help,” my friend said in frustration, “I wish they could make an appointment with those people. Ask THEM to explain so-called evidence behind their natural cures. I don’t know why they believe them and not me.”
Driving home, my friend’s words tumbled in my brain. I recalled conversations that I’ve had with well-meaning patients, caregivers and friends. It was true that many were not able to speak in person to those recommending “alternative” cures and I wondered if that was intentional on these influencer’s parts or just an added bonus. It is easy to say anything on social media, but more difficult to put your cards on the table and under the scrutiny of a desperate patient with cancer, explain the evidence behind your claims.
Why, I wondered, are physicians held to a higher standard? Not only am I morally and legally responsible for evidence-based practice, but I am also expected to explain why the opinions of non-scientific influencers are bunk. Where are these experts when patients have questions?
And where were they when patients who listened to them were harmed or even died by following their recommendations?
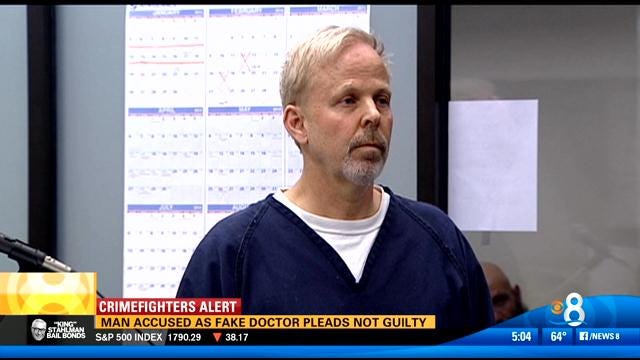
Instances of these deadly practitioners being held to account are rare. In 2018, for example, a jury ordered Robert O. Young to pay $105 million to a cancer patient.
Mr. Young is a naturopath who had persuaded the patient to forgo evidence-based treatment in favor of his alkaline diet. As a result of Mr. Young’s recommendations, the patient’s cancer progressed from curable to deadly. Mr. Young was defiant. Cancer, he said was not made up of abnormal cells, but an acidic poisonous liquid.
He was convicted. Twice. And spent time in jail.
Despite two convictions for practicing medicine without a license, his social media followings show his message is popular. He posts regularly on a YouTube channel (11,000 subscribers), Instagram (17,000 followers) and Twitter (40,000 followers). He also has over 60 books available for purchase on Amazon.
Unfortunately, Mr. Young is not alone. Researchers at Ohio State University studied popular cancer-related posts on TikTok. They found that the information - often in the form on emotional, first-person testimonials - was filled with inaccurate and dangerous misinformation.
So, is this non-vetted but readily available information helping patients make better decisions?
Unfortunately, no.
An analysis of the top 50 social media posts about common cancers found that audience engagement with posts that contained harmful information was almost double the engagement of fact-based posts.
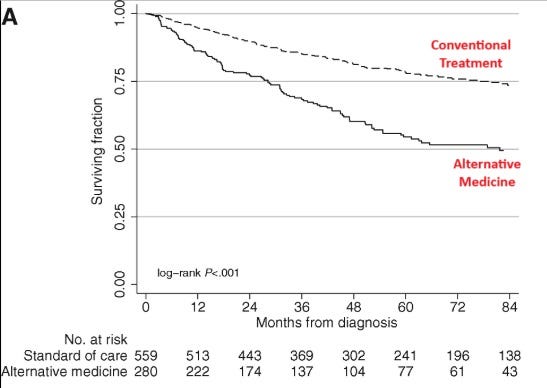
And this misinformation can be deadly. This study found that patients who choose alternative medicine as their sole anticancer treatment had double the rate of death compared to patients who follow conventional medical recommendations. In common cancers like breast, lung and colon, use of alternative medicine alone resulted in 5x as many patients dying of their disease.
Where are those numbers on social media?
In recent years, physicians have rightly been lauded for listening to their patients. For participating in shared decision-making instead of the patriarchal “doctor knows best” medicine that overshadowed the last century. Conversations about what outcomes matter to the patient have become more routine. I think we are getting better. Most of us are trying.
When I meet a patient for the first time, I have mere 60 minutes to cover ALOT of ground. I assume that patient believes that I am a qualified expert in my field. That based on thirteen years of training and twenty years of experience in seeing his or her type of cancer, I will tell them what I think is the best way forward to meet their goals.
If a patient wants talk about something they read online, that discussion takes time away from the part of medicine that I know best. That I would use to treat my loved one.
The cost of “doing your own research” may be less time spent hearing what the person who is willing to sit in front of you thinks.
To paraphrase Brene Brown, are you interested in the opinions of those who are not willing to be in the arena with us?
On my mind…
Thanks to all of you who have listened and shared Less Radical!
I’ve loved hearing your stories and memories. Keep ‘em coming! For those of you who haven’t listened yet, all six episodes are available now. It’s perfect binge listening for a weekend drive or upcoming holiday travel. We’ve been featured on NPR and The Guardian. A podcast insider called it a “remarkable story.”
Available on all podcast platforms or just click 👇.
Episode 1: Who is Bernie Fisher?
Our story begins exactly fifty years ago. On a fall weekend in late September 1974, a former dancer from Michigan and a young surgeon from Pittsburgh met just outside Washington, DC. The treatment of breast cancer would never be the same. Subscribe to Cancer Culture today and get all the episodes of Less Radical delivered directly to your inbox.






I’ve been playing Bob Seger for the last year. Such a great storyteller with an amazing voice!!
I always encourage ‘alternative’ breast cancer people to find out the cure and survival rates of patients with the same cancer from the ‘doctor’ before committing. It feels like some people just have a death wish . . .
I hope - if cancer ever knocks on my door - that I will have access to you. I can relate to snake oil salesmen and women 100% in my field (addiction and chronic non cancer pain). I came from a bit of a different side of “evidence” which was misinformation by docs and pharma to make money. I clearly remember the Porter and Jick “evidence” and watched pain specialists lapping up huge profits. Meanwhile I was lauded for “allowing my patients to suffer” for helping them get off of opioids, change lifestyle, help with the head shrinking traumas that exacerbated their pain, etc. Addiction and opioid induced hyperalgesia were poo pooed by many “experts” but understood when I saw the $ involved. I also saw “ultra rapid detox” as a thing. None of it worked and we see where we are with opioids of today.
In your case, however, denial in the patient became the tool of division - he wanted an easier softer way and went for it. Not your fault and certainly nothing you could say could convince him in any other way. I know how denial works and it’s a disease unto itself imo.
I sure appreciate you listing the conundrum you as the provider who KNOWS went through. It’s hard to see people smugly walking out the door to a likely miserable death. I saw it a lot over my career. The ones I remember today are the ones who came back and said, “Yeah, I think you might be right here and I’ll go thru what I need to.”
A clinician who does not bullshit or paint rosy pictures who is - HUMAN - is rare. I’m glad to know you are fighting this fight because you are clearly the right kind of doctor for such a terrible ordeal of treatment.